Clostridioides difficile (C. difficile) is a bacterium that can cause severe diarrhea and colitis. While naturally present in the environment and sometimes harmlessly residing in the human gut, C. difficile can proliferate and cause infection (CDI) when the gut’s natural microbial balance is disrupted, often due to antibiotic use. This article provides expert insights into CDI, covering its causes, symptoms, diagnosis, and current and future treatment options.
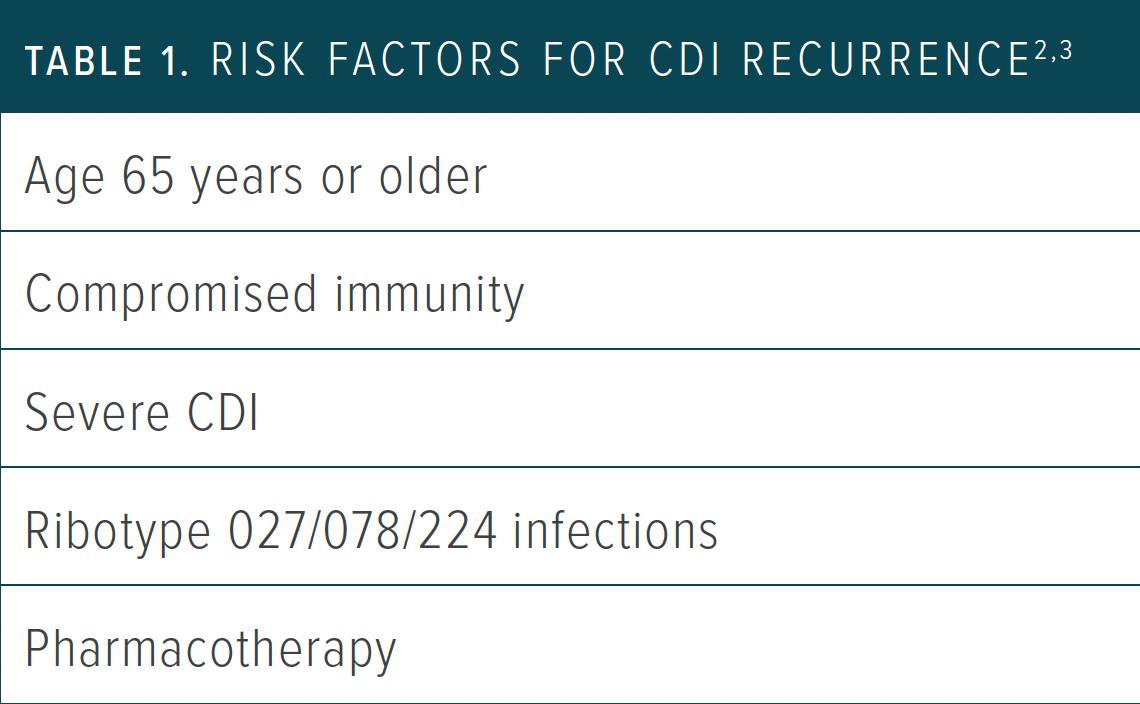 alt: Table illustrating risk factors for recurrent C. difficile infection, including antibiotic use, age, and underlying health conditions.
alt: Table illustrating risk factors for recurrent C. difficile infection, including antibiotic use, age, and underlying health conditions.
Understanding C. Difficile Infection
CDI is a significant concern, particularly among hospitalized patients and those over 65. The infection is primarily triggered by two toxins, TcdA and TcdB, produced by C. difficile. These toxins damage the colon’s lining, leading to inflammation and diarrhea. The rise of more virulent strains, like ribotype 027, has further complicated the fight against CDI.
How C. Difficile Spreads
C. difficile spreads through its resilient spores, which can persist on surfaces for extended periods. Transmission occurs via the fecal-oral route, often by touching contaminated surfaces and then ingesting the bacteria. Healthcare settings are particularly susceptible to outbreaks due to close patient proximity and frequent antibiotic use. Community-acquired CDI, not linked to hospitalization or antibiotics, is also increasing.
Recognizing the Symptoms of C. Difficile
CDI symptoms range from mild diarrhea and cramping to severe abdominal pain, fever, and dehydration. In severe cases, it can lead to life-threatening complications like toxic megacolon and pseudomembranous colitis. Some individuals may carry C. difficile without showing symptoms, unknowingly contributing to its spread.
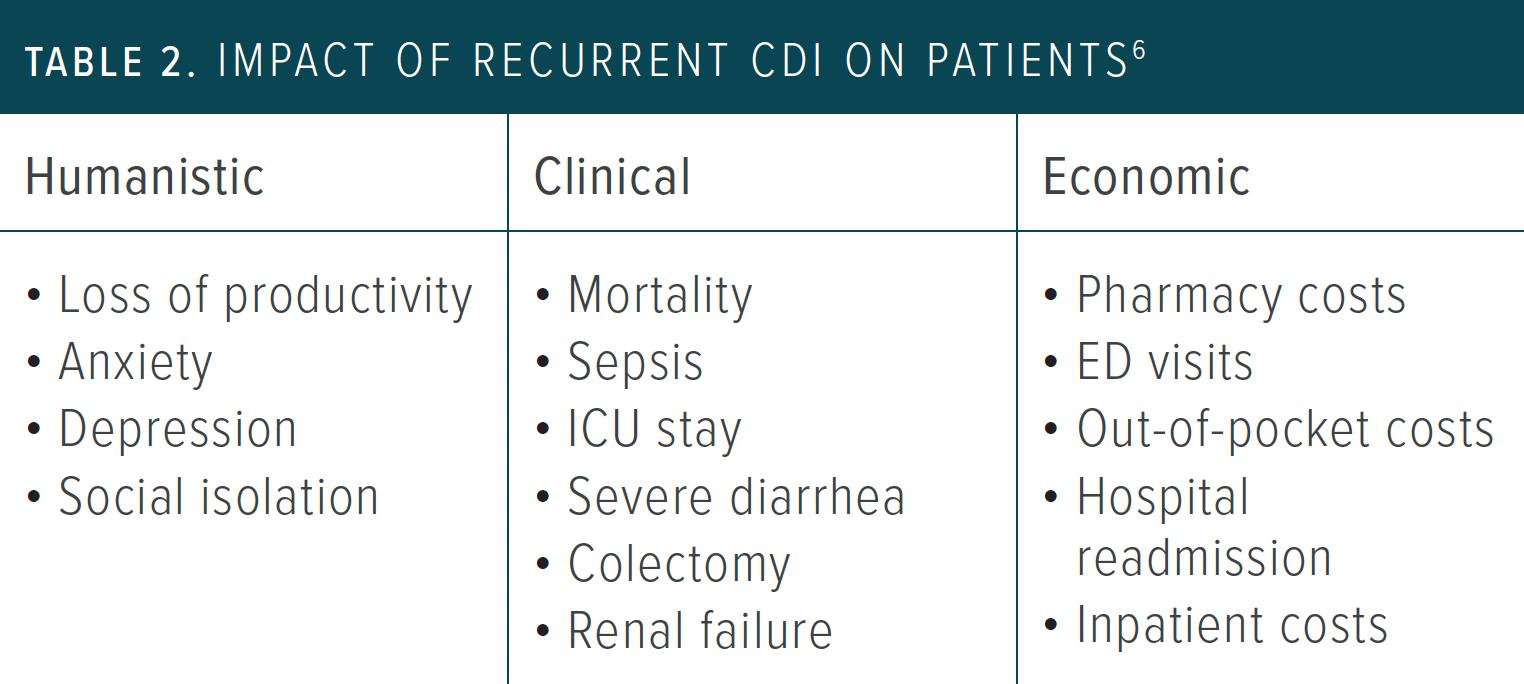 alt: Table highlighting the impact of recurrent CDI on patients, including hospital readmissions, emergency department visits, and decreased quality of life.
alt: Table highlighting the impact of recurrent CDI on patients, including hospital readmissions, emergency department visits, and decreased quality of life.
Diagnosing C. Difficile Infection
Diagnosing CDI involves assessing symptoms (three or more unformed stools within 24 hours) and confirming the presence of toxigenic C. difficile or its toxins through stool tests. Common laboratory tests include glutamate dehydrogenase (GDH), toxin enzyme immunoassay (EIA), and toxin B polymerase chain reaction (PCR).
Preventing C. Difficile Infection: Practical Advice
Handwashing with soap and water is crucial for preventing CDI transmission. Hand sanitizers are ineffective against C. difficile spores. Isolation of infected patients and thorough cleaning of contaminated surfaces with bleach-based products are essential.
Treatment Strategies for C. Difficile
Past Approaches
Early CDI guidelines primarily focused on initial treatment with metronidazole or vancomycin. However, these treatments had limitations, especially for recurrent infections.
Current Treatments
Current guidelines prioritize fidaxomicin for both initial and recurrent CDI, with vancomycin as an alternative. Bezlotoxumab, a monoclonal antibody targeting TcdB, is recommended for recurrent cases in high-risk patients. Fecal microbiota transplantation (FMT) offers a promising solution for multiple recurrences by restoring a healthy gut microbiome. FDA-approved FMT products, Rebyota and Vowst, are now available for preventing recurrent CDI.
Future Directions
Research into antibiotic resistance mechanisms is paving the way for novel therapies. Investigational drugs like RBX7455 and VE303 are undergoing clinical trials. Vaccines, like Pfizer’s PF-06425090, though currently halted, hold potential for future CDI management.
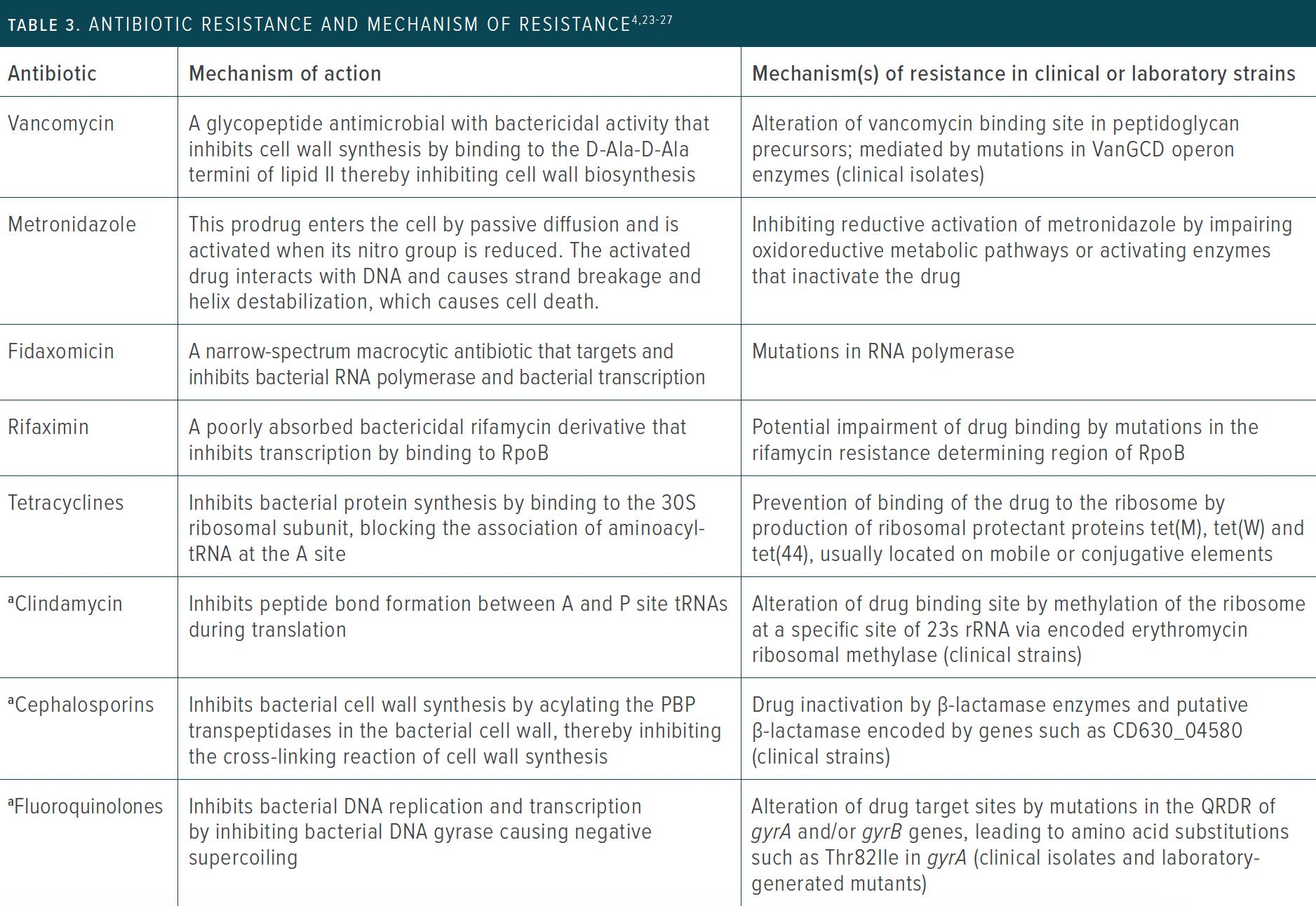 alt: Table detailing antibiotic resistance mechanisms in C. difficile, including alterations in penicillin-binding proteins, quinolone resistance-determining regions, ribosomal RNA, and transfer RNA. The table also lists antimicrobials associated with CDI.
alt: Table detailing antibiotic resistance mechanisms in C. difficile, including alterations in penicillin-binding proteins, quinolone resistance-determining regions, ribosomal RNA, and transfer RNA. The table also lists antimicrobials associated with CDI.
The Impact of Recurrent C. Difficile
Recurrent CDI significantly impacts patients’ lives, leading to physical discomfort, emotional distress, and reduced quality of life. Pharmacists play a vital role in managing CDI by optimizing treatment regimens, providing patient education, and promoting preventive measures.
Seeking Professional Guidance
For personalized treatment plans and further information on C. difficile infection, consult with a healthcare professional.

